Understanding Cancer Metastasis
- Moral Randeria

- Aug 1, 2025
- 3 min read
Updated: Sep 16, 2025
A summarized explanation of the key processes and methods by which cancer cells metastasis.
Introduction
Cancer Metastasis, occurs when cancer cells detaches from a primary tumor is and migrate to other parts of the body, creating new tumors. This aspect is the main cause of death and complications in cancer patients because it complicates treatment and disease management. The process of metastasis is intricate and involves multiple steps, including various biological and molecular shifts within the cancer cells and their exchanges with the nearby microenvironment.
Metastasis Morbidity
The World Health Organization (WHO) reports that cancer ranks as the second top cause of mortality worldwide, responsible for roughly 9.6 million deaths in 2018. It is estimated that metastatic cancers, rather than primary tumors, contribute to around 90% of these fatalities. Metastasis significantly contributes to pain, distress, and diminished quality of life by impacting crucial body parts like the brain, lungs, liver, bones, and lymph nodes. Patients with metastatic cancer usually face a bleak prognosis, and existing treatments tend to be palliative and limited in effectiveness. This underscores the critical need for a deeper comprehension of metastasis and the invention of more effective treatments and preventive strategies.
The Metastatic Cascade
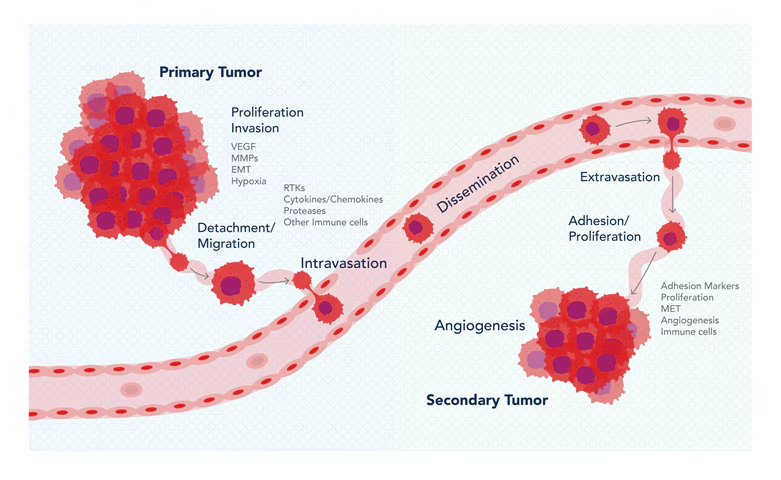
The metastatic cascade consists of six key steps: (1) local invasion, (2) intravasation, (3) circulation, (4) extravasation, (5) formation of micrometastasis, and (6) development of macrometastasis.
The metastatic journey of cancer cells includes a series of hurdles, including breaking away from the original tumor, enduring the conditions of the bloodstream, acclimating to new environments, and avoiding immune detection. A minority of the cancer cells that start metastasizing succeed in establishing noticeable secondary tumors, making metastasis an exceedingly inefficient and selective phenomenon.
The spread of cancer involves a process known as the metastatic cascade, where cancer cells follow a series of stages to establish themselves in another organ.
1. Invasion:
Cancer cells breach the basement membrane and extracellular matrix (ECM) encasing the original tumor, utilizing enzymes like matrix metalloproteinases (MMPs).
2. Intravasation:
Cancer cells infiltrate blood vessels or lymphatic channels, facing the forces of shear stress and immune system scrutiny.
3. Survival in bloodstream:
To persist in circulation, cancer cells have to withstand the bloodstream or lymphatic fluid's stringent conditions and dodge immune system assaults.
4. Arrest and extravasation:
Oncogenic cells attach to the endothelial cells lining the circulatory or lymphatic vessels and depart from the bloodstream via diapedesis or transendothelial migration.
5. Colonization:
Cancer cells modify themselves to fit into the unfamiliar microenvironment of a distant organ, beginning the development of micrometastases, which consist of tiny groupings of cancer cells that lack blood vessels.
6. Angiogenesis and Growth:
Cancer cells promote the generation of new blood vessels from pre-existing ones through angiogenesis, supplying oxygen and nutrients to the expanding micrometastases. The micrometastases grow and progress into macrometastases, which are tumors that can be detected through clinical methods.
The Molecular Mechanisms of Metastasis
The process of metastasis at the molecular level encompasses various changes in cancer cells and their relationship with the surrounding microenvironment.
Molecular Metastasis Mechanism:
1. Epithelial-mesenchymal transition (EMT):
EMT transforms epithelial cells, typically stationary and structured, into mesenchymal cells with greater movement and invasiveness. Triggered by elements like TGF-beta, EMT includes decreasing epithelial markers like E-cadherin and increasing mesenchymal markers such as N-cadherin and vimentin.
2. Cancer stem cells (CSCs):
Cancer stem cells (CSCs) refer to a subset of cancerous cells with capabilities for self-renewal and differentiation into diverse cell lineages. These cells exhibit increased resistance to standard treatments like chemotherapy and radiation and are more prone to causing metastasis. CSCs are distinguishable by the presence of particular surface markers, including CD44 and CD133.
3. Extracellular vesicles (EVs):
Extracellular vesicles (EVs) are compartments encapsulated by a membrane that cancer cells emit, containing diverse molecules including proteins, lipids, and nucleic acids. EVs can alter the actions of cancer cells and their surroundings, conveying cancer-promoting signals, bolstering new blood vessel growth, suppressing the immune response, and conditioning distant sites for metastasis.
4. Hypoxia:
Hypoxia is a state where oxygen levels are low within the primary tumor because it grows quickly and lacks proper blood vessels. This activates hypoxia-inducible factor (HIF), which controls genes that play a role in metastasis, including vascular endothelial growth factor (VEGF), CXCR4, and various MMPs.
5. Inflammation:
Inflammation acts as an immune mechanism reacting to infection or injury, which orchestrates a cascade of immune cells that include macrophages, neutrophils, and lymphocytes. This inflammatory process can accelerate metastasis through the secretion of pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-alpha), effectively promoting cancer cell growth, invasion, and longevity.
Reference
Siegel, R. L., Miller, K. D., & Jemal, A. (2019). Cancer statistics, 2019. CA: a cancer journal for clinicians, 69(1), 7-34.
Chaffer, C. L., & Weinberg, R. A. (2011). A perspective on cancer cell metastasis. Science, 331(6024), 1559-1564.

















Comments